What Exactly Causes Painful Heel
Overview
The plantar fascia is a thickened fibrous aponeurosis that originates from the medial tubercle of the calcaneus, runs forward to insert into the deep, short transverse ligaments of the metatarsal heads, dividing into 5 digital bands at the metatarsophalangeal joints and continuing forward to form the fibrous flexor sheathes on the plantar aspect of the toes. Small plantar nerves are invested in and around the plantar fascia, acting to register and mediate pain.
Causes
Plantar fasciitis generally occurs over time, rather than being the result of a single event. Micro trauma from repetitive stress to the tissue often combines with a biomechanical deficiency of the foot to produce the condition. In addition, arthritic and metabolic factors may contribute to the development of this injury, (though they are unlikely to affect young athletes). A variety of training errors commonly lead to plantar fasciitis, particularly a rapid increase in either volume or intensity of athletic activity. Volume refers to the distance or time an athlete performs, while intensity refers to the pace of activity and/or the recovery time allowed following performance.
Symptoms
When plantar fasciitis occurs, the pain is typically sharp and usually unilateral (70% of cases).Heel pain worsens by bearing weight on the heel after long periods of rest. Individuals with plantar fasciitis often report their symptoms are most intense during their first steps after getting out of bed or after prolonged periods of sitting. Improvement of symptoms is usually seen with continued walking. Numbness, tingling, swelling, or radiating pain are rare but reported symptoms. If the plantar fascia continues to be overused in the setting of plantar fasciitis, the plantar fascia can rupture. Typical signs and symptoms of plantar fascia rupture include a clicking or snapping sound, significant local swelling, and acute pain in the sole of the foot.
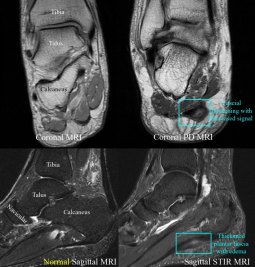
Diagnosis
Your GP or podiatrist (a healthcare professional who specialises in foot care) may be able to diagnose the cause of your heel pain by asking about your symptoms and examining your heel and foot. You will usually only need further tests if you have additional symptoms that suggest the cause of your heel pain is not inflammation, such as numbness or a tingling sensation in your foot, this could be a sign of nerve damage in your feet and legs (peripheral neuropathy) your foot feels hot and you have a high temperature (fever) of 38C (100.4F) or above – these could be signs of a bone infection, you have stiffness and swelling in your heel, this could be a sign of arthritis. Possible further tests may include blood tests, X-rays – where small doses of radiation are used to detect problems with your bones and tissues, a magnetic resonance imaging (MRI) scan or ultrasound scan, which are more detailed scans.
Non Surgical Treatment
You may experience concern in reading about treatment options for this condition that involve taking medications, having injections or undergoing surgery. While these remedies may be necessary in some cases, there are natural, non-invasive, affordable methods for treating and healing Plantar Fasciitis. A simple, three-step approach may be all you need to experience immediate or rapid symptom relief. Step 1) Give Your Feet A Rest. When a ligament is stressed and inflamed, it is absolutely essential to take pressure off it and let it rest. Adjust your daily habits to spend some time each day off your feet. Step 2) Ice Brings Cooling Relief. Apply an ice bag or cold pack to your heel for twenty minutes, twice a day. This will numb soreness and help control inflammation. Step 3) Gain Support From Orthotics. Orthotics are devices designed to modify body motions or lessen pressure on areas of the body. In the case of foot orthotics, these products may include splints, wraps and shoe inserts.

Surgical Treatment
Surgery is considered only after 12 months of aggressive nonsurgical treatment. Gastrocnemius recession. This is a surgical lengthening of the calf (gastrocnemius) muscles. Because tight calf muscles place increased stress on the plantar fascia, this procedure is useful for patients who still have difficulty flexing their feet, despite a year of calf stretches. In gastrocnemius recession, one of the two muscles that make up the calf is lengthened to increase the motion of the ankle. The procedure can be performed with a traditional, open incision or with a smaller incision and an endoscope, an instrument that contains a small camera. Your doctor will discuss the procedure that best meets your needs. Complication rates for gastrocnemius recession are low, but can include nerve damage. Plantar fascia release. If you have a normal range of ankle motion and continued heel pain, your doctor may recommend a partial release procedure. During surgery, the plantar fascia ligament is partially cut to relieve tension in the tissue. If you have a large bone spur, it will be removed, as well. Although the surgery can be performed endoscopically, it is more difficult than with an open incision. In addition, endoscopy has a higher risk of nerve damage.
Stretching Exercises
Stretching your plantar fasciitis is something you can do at home to relieve pain and speed healing. Ice massage performed three to four times per day in 15 to 20 minute intervals is also something you can do to reduce inflammation and pain. Placing arch supports in your shoes absorbs shock and takes pressure off the plantar fascia.